For nurses and healthcare workers, 12-hour shifts often mean being on your feet with little time for rest. Over time, this constant strain can lead to soreness, swelling, and even chronic foot problems.
The good news is that there are practical ways to prevent foot pain from standing, from choosing the right shoes and socks to stretching and recovery routines. A few consistent habits can protect your feet and help you feel less fatigued after every shift.
Why Standing All Day Causes Foot Pain
To effectively combat foot pain, one must first appreciate the multifaceted assault that prolonged standing wages on the human body. The aching, throbbing, and sharp pains are not random; they are direct physiological responses to intense mechanical, circulatory, and muscular stress.
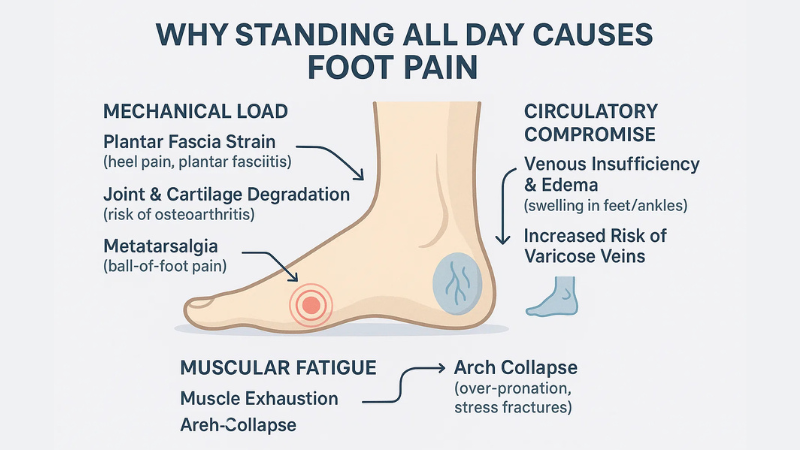
1. The Overwhelming Mechanical Load:
Your feet are a biomechanical masterpiece, containing a quarter of all the bones in your body, designed to adapt to varied terrain and absorb immense force. However, static standing locks this dynamic system into a state of relentless, unchanging pressure.
- Plantar Fascia Strain:
The plantar fascia, a thick, bowstring-like ligament that runs along the bottom of your foot from the heel to the toes, is crucial for maintaining the arch. During prolonged standing, this ligament is subjected to constant tensile stress, far exceeding its normal load.
This can lead to microscopic tears in the tissue, triggering an inflammatory response known as plantar fasciitis. This condition is characterized by sharp, stabbing pain in the heel, which is often most severe with the first steps in the morning.
If you are already suffering from plantar fasciitis and are in search for its remedies, don’t worry, we’ve got you covered. You can check out the natural remedies for plantar fasciitis to get rid of the condition.
- Joint and Cartilage Degradation:
The 33 joints in each foot are relentlessly compressed under your body weight. This constant pressure can wear down the protective cartilage that cushions the ends of your bones.
Over years, this can contribute to the development of osteoarthritis, a degenerative joint disease causing pain, stiffness, and reduced mobility.
- Metatarsalgia (Ball-of-Foot Pain):
Standing for hours, especially with a forward-leaning posture or in shoes with inadequate cushioning, places excessive pressure on the metatarsal bones at the ball of the foot. This can lead to inflammation and sharp, aching, or burning pain in this area, a condition known as metatarsalgia.
2. The Critical Circulatory Compromise:
Your circulatory system relies on movement to function efficiently. The muscles in your calves act as a powerful “secondary heart,” contracting and relaxing with each step to pump deoxygenated blood back up the legs towards the heart and lungs.
- Venous Insufficiency and Edema:
During static standing, this “calf muscle pump” is inactive. As a result, gravity takes over, causing blood and lymphatic fluid to pool in the lower extremities. This condition, known as venous pooling or stasis, leads to edema, or visible swelling in the feet, ankles, and lower legs.
This swelling increases internal pressure, compresses nerves, and is responsible for the common feeling of heavy, throbbing, and achy legs.
- Increased Risk of Varicose Veins:
Over time, chronic venous pooling can increase the pressure on the veins in your legs, damaging the tiny one-way valves that prevent blood from flowing backward. This can lead to the development of painful, bulging varicose veins.
3. The Inevitable Muscular Fatigue:
The dozens of small, intrinsic muscles within your feet are responsible for fine motor control, balance, and providing dynamic support to your arches.
- Muscle Exhaustion and Arch Collapse:
Like any muscle under constant tension, these intrinsic foot muscles eventually become exhausted. As they fatigue, they can no longer effectively support the arch, causing it to flatten (a condition known as over-pronation).
This transfers the entire load of supporting your body weight onto your ligaments and bones—structures not designed for this purpose—leading to widespread pain and increasing the risk of stress fractures.
Foot Care Checklist to Prevent Foot Pain from Standing All Day
Creating a structured routine is the most effective way to build resilience against foot pain. This checklist breaks down the essential actions into manageable steps to be performed before, during, and after your shift.
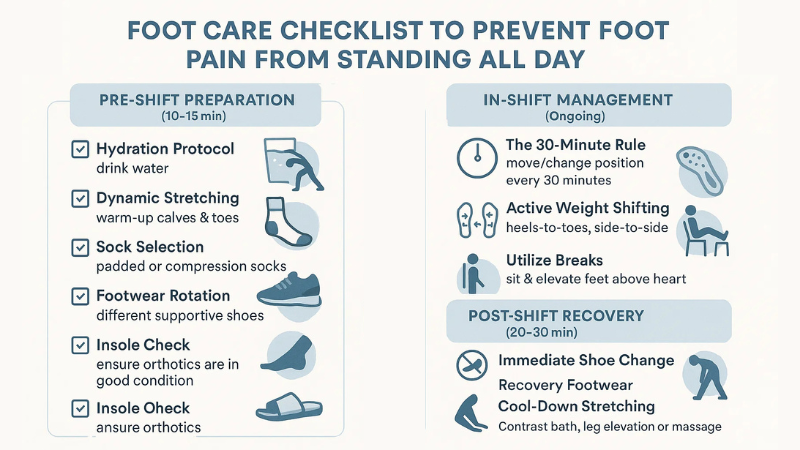
Pre-Shift Preparation (10-15 minutes):
- Hydration Protocol:
Begin hydrating before your shift starts. Drink a large glass of water to ensure your muscles and connective tissues are well-hydrated.
- Dynamic Stretching Routine:
Perform the full 5-10 minute pre-shift stretching circuit detailed below to warm up your calves, arches, and toes.
- Sock Selection:
Choose your socks strategically.
- Padded Socks: For days when you anticipate more standing on hard surfaces, select socks with extra cushioning in the heel and forefoot.
- Compression Socks (15-20 mmHg): For days involving more walking or if you are prone to swelling, choose moderate compression to promote circulation.
- Footwear Rotation:
Select a different pair of supportive work shoes from your rotation. This guarantees the foam midsole has had at least 24 hours to decompress and restore its full cushioning capacity.
- Insole Check:
Ensure your orthotic insoles are positioned correctly and are not showing signs of excessive wear (e.g., thinning, cracking).
In-Shift Management (Ongoing):
- The 30-Minute Rule:
Set a mental or actual timer to remind yourself to change your position or move every 30 minutes. Even a 60-second “movement snack” can make a huge difference.
- Active Weight Shifting:
Consciously practice shifting your weight. Rock gently from heels to toes, side to side. If possible, prop one foot up on a low stool or rail for a few minutes, then switch.
- Utilize Break Time Wisely:
During your designated breaks, prioritize getting off your feet. Find a quiet place to sit and elevate your feet on another chair or stool, aiming to get them above heart level to let gravity assist with fluid drainage.
- Maintain Proper Posture:
Keep your core engaged, shoulders back, and head level. This ensures your weight is distributed evenly across both feet, preventing overload on any single part.
Post-Shift Recovery (20-30 minutes):
- Immediate Shoe Change:
The moment you get home, remove your work shoes and socks. Let your feet breathe.
- Switch to Recovery Footwear:
Slip into dedicated recovery sandals or supportive slippers. Walking barefoot on hard floors can continue to strain your feet.
- Cool-Down Stretching:
Perform a gentle 5-minute stretching routine to release the tension built up over the day.
- Implement a Recovery Protocol:
Choose one of the deep recovery methods detailed later (e.g., contrast bath, leg elevation, deep tissue massage) and dedicate at least 15 minutes to it. You can also get a post shift foot massage to get relaxed.
How to Stretch Feet Before a 12-Hour Shift to Prevent Foot Pain From Standing
This pre-shift warm-up is non-negotiable. It primes the muscles and connective tissues for the long day, significantly reducing the risk of strain and injury.

1. Deep Calf Stretches (Two Positions):
- Gastrocnemius Stretch:
Stand facing a wall with your hands on it for support. Step your right foot back about 2-3 feet, keeping your heel firmly planted on the floor and your back leg straight.
Gently bend your front knee and lean your hips forward until you feel a strong stretch in the upper part of your right calf. Hold this position for a full 30 seconds, breathing deeply.
- Soleus Stretch:
From the previous position, slightly bend your back (right) knee while keeping your heel on the floor. You will feel the stretch move lower down your calf, closer to the Achilles tendon.
This targets the soleus muscle, a key player in ankle stability. Hold for another 30 seconds. Repeat both stretches on the left leg.
2. Seated Plantar Fascia Stretch:
Sit comfortably in a chair. Cross your right ankle over your left knee. With your right hand, grasp all five toes of your right foot and gently pull them back toward your right shin.
You should feel a distinct, pleasant stretch along the entire arch of your foot. Use your left thumb to massage the arch while it’s stretched. Hold for 30 seconds. Repeat 3 times on each foot.
3. Self-Myofascial Release with a Ball:
While seated, place a tennis ball, lacrosse ball, or a specialized foot roller under your right foot. Slowly roll the ball from your heel to the ball of your foot, applying consistent, moderate pressure. When you find a particularly tender spot, pause your rolling and hold the pressure on that spot for 20-30 seconds to help the muscle release.
This helps break up knots and improve circulation. Spend at least 1-2 minutes on each foot. A frozen water bottle can be used to combine this with cold therapy.
4. Towel Scrunches and Toe Splaying:
Sit with your feet flat on the floor and place a small hand towel in front of you. Using only your toes, try to scrunch the towel and pull it toward you.
Then, reverse the motion and push it away. This strengthens the intrinsic muscles of the foot. Follow this by practicing “toe splaying”—actively trying to spread your toes as wide apart as possible, then relaxing. Repeat 10-15 times.
Best Ways to Manage Foot Pressure at Work
While you’re on the clock, these active strategies can help redistribute pressure and fight off fatigue.
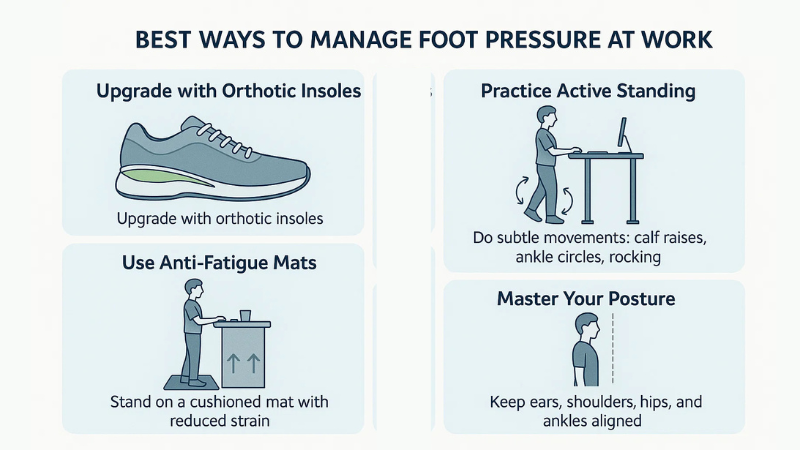
- Upgrade with High-Quality Orthotic Insoles:
Factory insoles provided with shoes are often flimsy pieces of foam offering little to no real support. Investing in a quality pair of over-the-counter or custom orthotics is a game-changer.
Look for insoles with a semi-rigid arch support to prevent collapse, a deep heel cup for stability, and a top layer of memory foam or poron for superior shock absorption. This simple addition can transform a good shoe into a great one.
- Practice Active Standing:
Static standing is the enemy. Turn your standing into a dynamic activity. In addition to shifting your weight, perform subtle, almost invisible movements.
Do a few calf raises while waiting for a document to print. Do some ankle circles while on the phone. Rock back and forth. These micro-movements are enough to keep your calf muscle pump engaged and blood flowing.
- Advocate for Anti-Fatigue Mats:
If your primary workspace is a fixed location (like a medication dispensing station, a lab bench, or a checkout counter) and does not have an anti-fatigue mat, speak with your manager or occupational health department.
Present it not as a personal comfort request, but as a proven workplace safety measure that can reduce musculoskeletal injuries and improve employee productivity and well-being.
- Master Your Posture:
Think of a string pulling you up from the crown of your head. Align your ears over your shoulders, shoulders over your hips, and hips over your ankles.
Engage your core muscles to support your spine. This alignment ensures your body weight is distributed evenly, not just between your feet, but across the entire surface of each foot, preventing pressure hotspots.
Choosing the Right Footwear for Long Shifts
Your shoes are the most critical tool in your arsenal against foot pain. Making an informed choice is paramount.

- Cushioning is King:
The midsole of the shoe is its engine. Look for shoes with thick, responsive midsoles made from high-quality materials like EVA foam, Polyurethane (PU), or proprietary technologies (e.g., Hoka’s ProFly, Brooks’ DNA Loft).
The ideal cushioning is a balance—soft enough to absorb impact but firm enough to provide a stable platform.
- The Toe Box Test:
Before buying, take out the shoe’s insole and stand on it. Your entire foot should fit on the insole without your toes or the ball of your foot spilling over the sides. If it spills over, the toe box is too narrow, which will lead to cramping, bunions, and nerve compression.
- Arch Support & Torsional Stability:
A supportive shoe should not be able to bend or twist easily in the middle. Pick up the shoe and try to twist it like you’re wringing out a towel. There should be significant resistance. This torsional stability prevents your foot from over-pronating and protects your arch.
- The “Rule of Thumb”:
There should be about a thumb’s width (about half an inch) of space between your longest toe and the end of the shoe. This allows your foot to expand naturally throughout the day without your toes hitting the end of the shoe.
- Zero-Drop vs. Traditional Heel:
Consider the heel-to-toe drop. Traditional running shoes have a significant drop (8-12mm), while some brands offer “zero-drop” or low-drop options.
A lower drop can promote a more natural midfoot strike but requires a transition period for your calves and Achilles to adapt. Experiment to see what feels best for your body mechanics.
Daily Recovery Tips for Nurse Foot Fatigue
Recovery is not a luxury; it’s a necessity. This is when your body repairs the micro-damage from the day.

- Epsom Salt Soaks:
Magnesium sulfate (Epsom salt) is known to help relax muscles and reduce inflammation. Fill a basin with warm water (not hot, as that can sometimes increase inflammation) and add a generous cup of Epsom salt. Soaking for 15-20 minutes can provide immense relief to sore, aching muscles.
- Cryotherapy (Ice Massage):
For acute pain, especially heel pain from plantar fasciitis, ice is your best friend. Freeze a water bottle and roll it under your arch for 10-15 minutes. This combines the benefits of massage with cryotherapy to numb pain and constrict blood vessels, reducing inflammation and swelling.
- Elevate Your Legs Effectively:
The “Legs-Up-the-Wall” pose is the gold standard. Lie on your back and scoot your hips as close to a wall as possible, resting your legs straight up against it.
This uses gravity to its full advantage, draining excess fluid from your legs and feet far more effectively than simply propping them on pillows. Stay in this position for 10-15 minutes while you relax, listen to music, or practice deep breathing.
How to Reduce Foot Pain From Standing All Day After Long Shifts
These long-term habits will build resilience and manage the cumulative effects of standing day after day.

- The Power of Footwear Rotation:
The foam in your shoe’s midsole is made of tiny gas-filled cells that get compressed with every step. It can take 24-48 hours for these cells to fully reinflate and regain their original cushioning properties.
By rotating between at least two pairs of high-quality work shoes, you ensure you are always starting your shift with a fully functional shock absorption system.
- Embrace Recovery Footwear:
The concept of recovery footwear is based on providing maximum cushioning and arch support to offload the stressed tissues in your feet. Brands like OOFOS and Hoka have created sandals and slides with oversized, rockered soles and significant arch support.
Wearing these around the house gives your feet a supportive, cushioned environment in which to heal.
- Hydration and Anti-Inflammatory Diet:
Chronic, low-grade inflammation can make you more susceptible to foot pain. Fight it from the inside out. Drink plenty of water to help flush out metabolic waste.
Focus your diet on whole foods rich in anti-inflammatory properties: fatty fish (salmon, mackerel), nuts (walnuts, almonds), seeds (flax, chia), fruits (berries, cherries), and leafy green vegetables. Limit pro-inflammatory foods like processed sugars, refined carbohydrates, and fried foods.
Recommended Products (Affiliate Section)
Investing in the right tools can significantly enhance your comfort and accelerate your recovery. Professionals who stand all day often see tremendous benefits from:
Products | Specialities | |
Foot Rollers | For targeted deep tissue self-massage to release knots in the plantar fascia and intrinsic foot muscles. | |
Massage Balls | For targeted deep tissue self-massage to release knots in the plantar fascia and intrinsic foot muscles. | |
Compression Socks | To combat swelling and improve circulation throughout the workday. | |
Podiatrist Approved Orthotic Insoles | To provide customized arch support and superior cushioning inside your work shoes. | |
Dedicated Foot Pain Recovery Sandals | For providing a cushioned, supportive environment for your feet at home post-shift. |
Conclusion
Preventing foot pain from standing all day is an active, ongoing process that requires dedication and a multi-pronged strategy. It is not about finding a single cure, but about building a resilient system of support for your body’s foundation.
By diligently warming up with targeted stretches, making an informed and uncompromising choice in your footwear, and actively managing pressure throughout your shift, you can take control of your foot health.
These practices are an investment in your career longevity, your daily comfort, and your overall well-being. By treating your feet with the care and respect they deserve, you can ensure they continue to support you reliably and pain-free through every long shift.
FAQs About Preventing Foot Pain from Standing All Day
What’s the best way to prevent foot pain from standing all day?
The best way is a combination of four key elements: wearing highly supportive, well-cushioned shoes; using compression socks or padded socks; performing daily stretching routines for your feet and calves; and practicing a consistent post-shift recovery routine like soaking or massage.
How do nurses deal with sore feet?
Experienced nurses often use a multi-faceted approach. They invest in premium footwear and rotate pairs, wear compression socks to manage swelling, take short breaks to stretch and shift weight, and have a dedicated at-home recovery plan that often includes Epsom salt soaks, foot massages, and leg elevation.
Are compression socks good for standing all day?
Yes, they are exceptionally beneficial. They apply gentle, graduated pressure to the legs, which helps prevent blood and fluid from pooling in the feet and ankles. This significantly reduces swelling, aching, and the feeling of heavy, tired legs.
What stretches help with foot pain before and after work?
The most effective stretches are deep calf stretches (both with a straight and bent knee), seated plantar fascia stretches (pulling toes toward the shin), and rolling the arch of the foot over a tennis or massage ball to release tension.
How often should I replace shoes if I work 12-hour shifts?
As a general rule, shoes worn for long shifts should be replaced every 6 to 9 months, or after 300-500 miles of use. Signs that it’s time for a replacement include visible creasing and compression in the midsole foam, worn-down tread, and a noticeable decrease in cushioning and support.

Leave a Reply